
Researchers from the Royal Women’s Hospital joined leading international experts to share the latest in newborn medicine at the annual Cool Topics conference last week.
Hosted by the Royal Women’s Hospital, over 200 clinicians from Australia and New Zealand gathered to learn the latest best-practice care for sick or premature babies.
Over two days, there were 20 presentations and in-depth panel discussions. Topics covered all aspects of medical interventions to help babies thrive as children and as adults.
The conference also had a strong focus on the lived experience of parents of preterm babies ... and how to best involve them in shared decision-making.
This is a particularly sensitive issue when questions around end-of-life care need to be discussed.
Dr Sid Vemuri is a palliative care physician who works in the Victorian Paediatric Palliative Care Program. In his research, he identified and coined the term "shepherding" for a previously unrecognised communication behaviour.
"Shepherding is a subtle process. It gently guides parents to understand their child's health and potential suffering before they make decisions," Dr Vemuri said.
“Shepherding leaves space for parents’ own thinking. It does not guarantee that parents will think as paediatricians hope. Nor that they will make treatment decisions that paediatricians prefer.”
Facing these conversations is the most gruesome and heartbreaking experience as Samantha O’Dwyer explained.
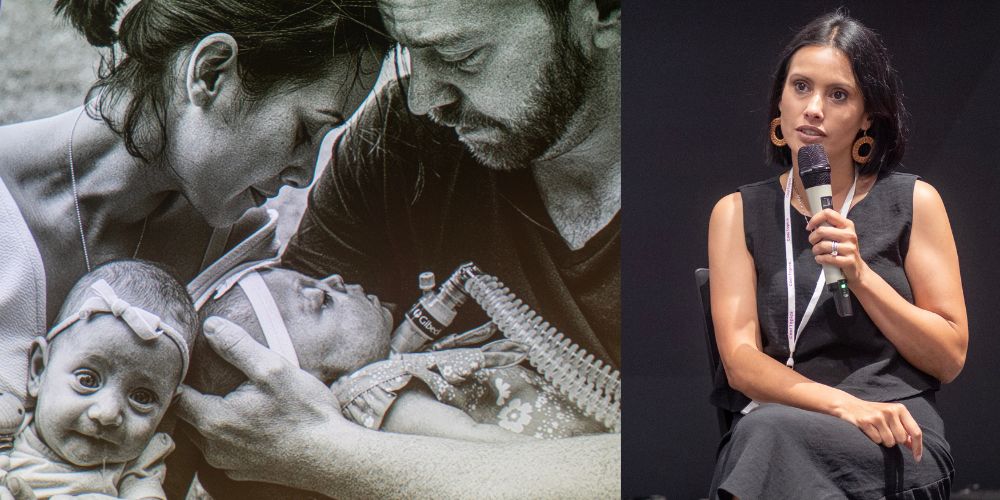
Samantha is a mother of five. At Cool Topics, she shared her journey as a bereaved mum to Nora, her “medically complex NICU warrior.”
Nora was born at 28 weeks. She weighed 960 grams and faced many serious health challenges. Despite numerous surgeries and life-threatening conditions, Nora's resilience and the love from her family and medical team kept them hopeful.
However, after a severe cold, Nora's health worsened. The family decided to stop resuscitation efforts and, after several days of rapid decline, eventually chose for Nora to be made comfortable while they had one last magical day to say goodbye.
Samantha explained that it really matters how medical staff approach difficult conversations.
She recalled a particularly upsetting example. One well-meaning doctor had gone too far and explained that Nora had less than a 20 per cent chance of surviving the week.
“I knew this doctor thought she was helping me to better understand the dire situation in which we found ourselves,” Samantha said.
“But at that moment, alone in a hospital room with my seriously ill child, I wasn't in any position to hear this.”

Maggie Lloyd is another mum of a 27-week preterm baby who shared her NICU experience at Cool Topics.
Unlike Samantha, Maggie was lucky to bring her baby home. Her daughter Jasmine is now 23 years young.
Yet, Maggie shared that getting to this point was anything but easy.
Jasmine developed various health complications from being born too early. Despite initial progress, Jasmine faced behavioural difficulties. Eventually, she was diagnosed with mental health conditions and sensory processing disorder.
Maggie is a passionate advocate for better support for parents of preterm babies.
“We're so grateful to all the neonatologists and researchers because we've still got a great outcome,” Maggie said.
"I only wish there was more out there ... more information and resources for us to give to various health professionals and teachers. They need to know how to better support children born too early."
“If only all health professionals, GPs, kinder and school teachers were educated on how to better support children born too early.”